Adult Emergency Medicine Guide
Procedures
Lumbar Puncture
Cerebral Spinal Fluid Orders
Tubes 1 & 4: Cell Count and Differential
Tube 2: Glucose and Protein
Tube 3: Gram Stain and Culture
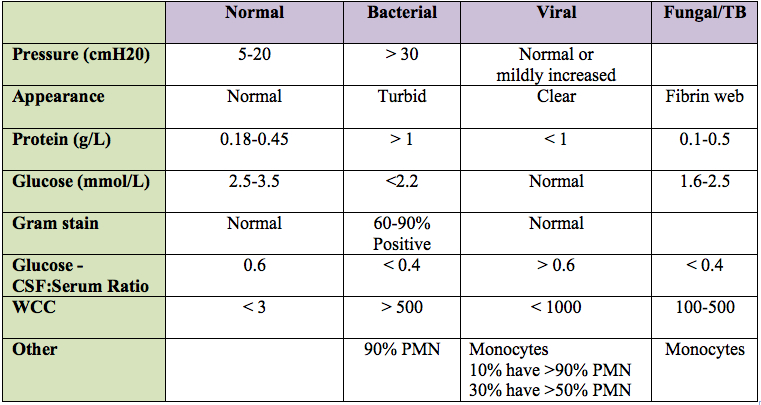
Lumbar Puncture Results Interpretation
Arthrocentesis
Arthrocentesis Synovial Fluid Orders
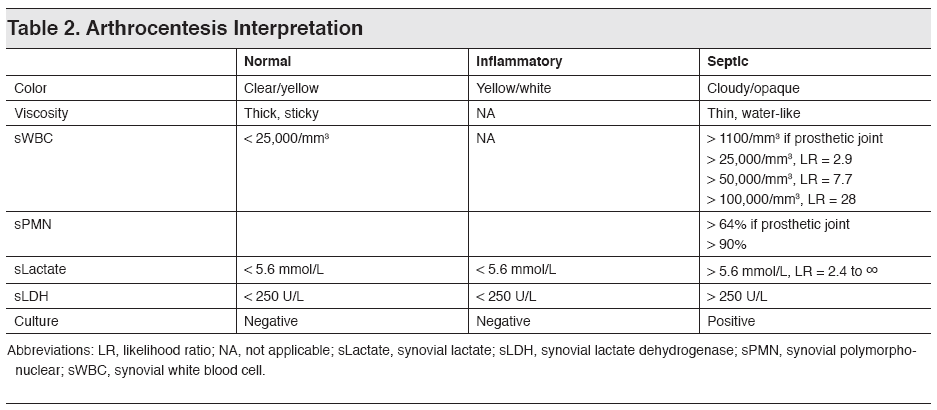
Results Interpretation
HEENT
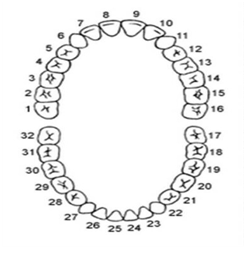
Adult Dental Chart
Musculoskeletal
Code Cord Compression
Algorithm for Management of Non-Traumatic Back Pain
Consider these Red Flags for possible cord/cauda equina compression to determine appropriate pathway
History
Epidural abscess: fever, immunocompromised, IVDA, history of bacteremia
Epidural tumer: history of cancer or weight loss
Epidural hematoma: anticoagulation, recent spinal anesthesia
General: new frequent falls or ataxia, greater than 3 weeks of midline pain, nocturnal pain, sphincter incontinence or urinary urgency, bilateral leg symptoms
Physical Exam
Motor: weakness in legs (or arms)
Sensory: sensory level or saddle anesthesia
Reflexes: diminished or abnormal reflexes, including positive (upward) Babinski reflex
Sphincter tone: lax rectal tone (rectal should be performed on intermediate or high risk patients), post-void residual greater than 100mL
Low Risk
No red flags and normal neurologic exam (or isolated single root finding consistent with sciatica)
- No routine lab testing, imaging, or consults.
- Treat symptoms:
- Use non-steroidal anti-inflammatory drug; opioids for severe pain.
- Consider a muscle relaxant.
- Bedrest for 2-3 days for severe pain.
- Rapid return to normal activities.
- Explain problem and treatment to patient.
- Follow-up with PCP.
- Provide written instructions about symptoms requiring return visit (including red flags)
Intermediate Risk
Presence of one or more red flags and normal neurologic exam (or isolated single root finding consistent with sciatica)
Consider (case-by-case)
- Empiric antibiotics
- Empiric IV dexamethasone
- Consult spine surgery
Options based on clinical judgement:
- Further risk stratification: CRP or ESR for possible cancer or spinal abscess.
- Consult neurology or spine surgery.
- Consider imaging:
- Emergent MRI in the ED?
- Urgent MRI as outpatient in 48 hours?
- Disposition
- Discharge with urgent MRI and PCP follow-up?
- Admission or observation in hospital?
CAUTION!
- Communicate clearly with patient:
- About plans, concerns, and need for PCP follow-up.
- Symptoms requiring return to the ED.
- Coordinate with PCP or admitting provider.
- Treat symptoms in analgesics.
High Risk
Any new abnormality on neurologic exam (except for isolated single root finding consistent with sciatica)
- Empiric antibiotics
- Empiric IV dexamethasone
- Consult spine surgery
Emergency MRI
Initiate rapid imaging of the correct portion of the spine.
Positive MRI
- Start ED-based treatments and/or consultations based on the diagnosis.
- Consult spine surgeon for definitive care.
- Review MRI with radiologist:
- Is the scan truly negative?
- Is the scan technically-adequate?
- Have the correct levels been imaged?
- Repeat the neurologic exam:
- Is it truly abnormal?
- Has it evolved?
- Consider lumbar puncture.
- Admit or observe for further evaluation.
FOR HIGH RISK (AND APPROPRIATE INTERMEDIATE-RISK) CASES:
- Determine imaging level based on exam findings and possible diagnosis:
- If spinal epidural abscess or metastatic cancer is a concern, the entire spine should be imaged because skip areas with abscess or multiple metastasis are common.Discuss case with radiologist, including need for emergent MRI.
- Use Primordial Communicator or call x7-7076.
- After-hours, call teleradiologist at (877)595-1271.
- Order MRI and notify imaging about STAT order at x7-7007.
- Ensure pain and anxiety are well controlled, using weight-based analgesic doses.
- Consider empiric antibiotics (after cultures) and IV dexamethasone.
- Consider notifying neurosurgeon at (410)391-6904.
Cord Compression Imaging Protocol
- CPOE order for “STAT-CORD COMPRESSION MRI” will be placed by referring physician. Embedded screening questions in MedConnect including suspected reason for cord compression and suspected sensory/motor level will be required to activate this order. This order should include a prompt to call radiologist.
- Referring physician will call radiologist and discuss whether this is an appropriate exam, if sedation or general anesthesia will be required, or if another exam such as CT myelography is indicated.
- Radiologist will call MRI department.
- All sites should have a specific abbreviated cord compression protocol including Sag T1, T2 and STIR of cervical and upper thoracic spine followed by Sag T1, T2 and STIR of lower thoracic and lumbar spine on all scanners.
- This should be a non-contrast exam to reduce the scan time.
- If available, 3D T2 weighted sagittal images (T2 SPACE or equivalent) enable obtaining reformatted axials through the entire spine. Otherwise axial T2 weighted images can be obtained through selected levels if needed.
- Technologist will contact radiologist when the study is completed. Some sites may elect to have the radiologist notified while the patient is still on the scanner so that the radiologist can add additional sequences.
- Radiologist will give preliminary interpretation within 30 minutes of completion.
- Radiologist must call the referring physician WHETHER OR NOT the study is positive.
- Radiologist will document communication.
- If MRI is unsuccessful, radiologist will discuss the need for alternative imaging, including CT myelography, with referring physician.
- If this is not available on site, then patient will be transferred to a facility where this is available
- Results of CT myelography will be called to referring physician within 30 minutes of completion.
- All cord compression imaging studies will be tracked, ideally with an automated dashboard linked to the specific CCP order in MedConnect.
- Items tracked should include time of order, time completed, and time result is called.
Sepsis
Sepsis Cheat Sheet
Severe Sepsis
All three of the following must be met within 6 hours of each other.
- Documentation of a suspected source of clinical infection.
- Two or more manifestations of systemic infection according to
the SIRS criteria, which are:
- Temperature > 38.3 or < 36.0 C
- Heart rate > 90
- WBC > 12K or < 4K or > 10% bands
- Respiratory rate> 20
- Organ dysfunction, evidenced by any one of the following:
- SBP < 90, or MAP < 65, or a SBP decrease of more than 40 pts
- Cr > 2.0, or urine output < 0.5 mL/kg/hour for 2 hours
- Bilirubin > 2 mg/dL (34.2 mmol/L)
- Platelet count < 100,000
- INR > 1.5 or a PTT > 60 sec
- Lactate > 2 mmol/L (18.0 mg/dL)
Septic Shock
The criteria for Septic Shock are:
- Severe Sepsis
AND
- Tissue hypoperfusion persists in the hour after
crystalloid fluid administration, evidenced by either
▪ Continued hypotensionOR
▪ Lactate level is >= 4 mmol/L
Treatment
0-3 hour bundle
- Obtain lactate
- Obtain blood cultures before initiation of antibiotics
- Broad spectrum antibiotics administered (see bottom of page for suggested antibiotic coverage)
- Administer 30ml/kg IVF bolus
3-6 hour bundle
- Persistent hypotension or lactate >4, assess volume status and tissue perfusion (see box below for documentation)
- Repeat lactate level to be drawn after IVF bolus of 30 ml/kg
- Initiate vasopressors to maintain MAP >65 after 30 ml/kg IVF bolus
A focused exam performed by physician/APN/PA including all:
▪ Vital signs review ,
▪ Cardiopulmonary exam,
▪ Capillary refill evaluation,
▪ Peripheral pulse evaluation,
▪ Skin examination
Any two of the following four:
▪ Bedside Cardiovascular Ultrasound (echo, trans-thoracic echo, TTE, TEE, IVC ultrasound, 2D echo, Doppler echo, Echocardiogram with Doppler, Doppler US of the heart)
▪ Passive Leg Raise Exam by physician/APN/PA or Fluid Challenge given
▪ Central venous pressure measurement (CVP or RAP/right atrial pressure)
▪ Central venous oxygen measurement (SVO2, ScvO2 or oxygen saturation via central catheter)
Broad Spectrum Antibiotics
[table]
Infection,Primary Therapy, Alternate for Beta-Lactam Allergy
Pneumonia (CAP),Ceftriaxone 1g IV Q24 + Azithromycin 500 IV Q24, Levofloxacin 750 IV Q24
Pneumonia (HCAP), Cefepime 1g IV Q8 + Azithromycin 500 IV Q24+ Vancomycin IVPB** 2nd antibiotic given**, Aztreonam 2g IV Q8+ Levofloxacin 750 IV Q24+ Vancomycin IVPB**2nd antibiotic given**
Urinary,Cefepime 1g IV Q8H, Aztreonam 2g IV Q8
CNS,Ceftriaxone 2g IV Q12+ Vancomycin IV+
Ampicillin 2g IV Q4 (age>50), Meropenem 2g IV Q8+
TMP/SMX 5mg/kg IV Q6+
Vancomycin IVPB **2nd antibiotic given**
Intra-abdominal, Piperacillin/Tazobactam 4.5g IVq8h, Levofloxacin 750mg IV q24 + Metronidazole 500mg IV q8 + (Vancomycin IVPB) **2nd given**
[/table]