Pediatric Emergency Medicine Guide
Vital Signs
Rapid Assessment and Vital Signs
MedStar Pediatric Emergency Medicine Clinical Practice Council
Pediatric Rapid Assessment
Responsiveness: GCS, tone, activity
Airway: Patent, maintainable with positioning, unmaintainable
Breathing: Respiratory rate, work of breathing, color, breath sounds, pulse ox
Circulation: Heart rate, capillary refill time, skin color and temp, central vs peripheral pulses, LOC
Pediatric Parameters
[table class=”table-striped”]
Age, Wt (kg),HR,RR,SBP
Newborn, 3.5,130,40,70
3 mo,6,140,30,80
6 mo, 8,130,30,80
1 yr, 10,120,26,90
2 yr, 12,115,26,90
3 yr, 15,110,24,90
4 yr, 17,100,24,90
6 yr, 20,100,20,95
8 yr, 25,90,20,95
12 yr, 40,85,20,105
[/table]
*Hypotension= Systolic BP less than or equal to 70 + (2 x age in years over 1 year)
Fluid Resuscitation and Urine Output
Fluid Resuscitation
IV FLUID RATES & URINE OUTPUT
Maintenance IV Fluids
~For kids <10kg:
100 mL/kg/day
~For kids >10kg:
4 mL/kg /hr for the first 10 kg
2 mL/kg/hr for the next 10 kg
1 mL/kg/hr for every kg >20 kg
Urine Output
Normal 1-2 mL/kg/hr
Minimum 0.5-1 mL/kg/hr
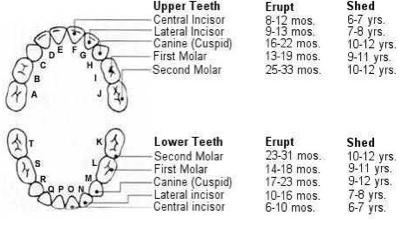
HEENT
Pediatric Dental Chart
Abdomen
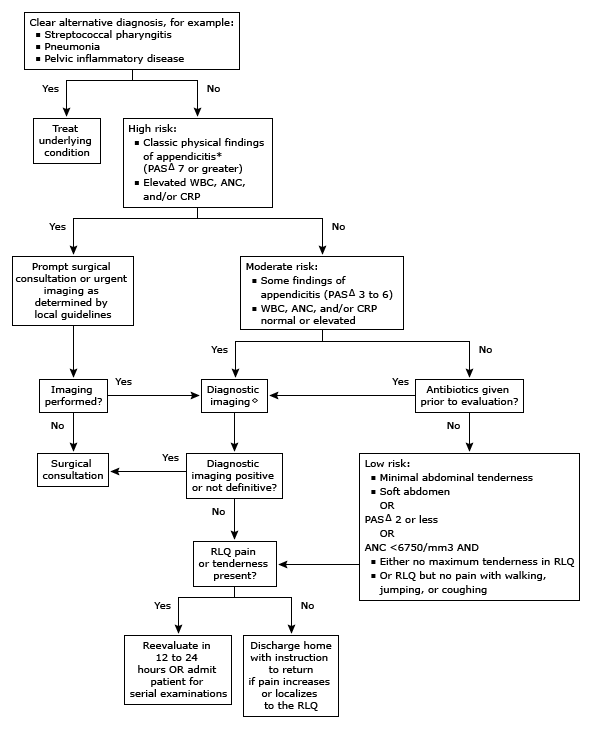
Acute Appendicitis
Anatomy: The appendix arises from the cecum, which is located in the right lower quadrant of the abdomen in the majority of children.
It may lie in the upper abdomen or on the left side in children with congenital abnormalities of intestinal position, situs inversus totalis, and after repair of diaphragmatic hernia, gastroschisis, and omphalocele.
The classic presentation of appendicitis includes the following clinical findings:
- Anorexia
- Periumbilical pain (early)
- Migration of pain to the right lower quadrant (often within 24 hours of onset of symptoms)
- Vomiting (typically occurring after the onset of pain)
- Fever (commonly occurring 24 to 48 hours after onset of symptoms)
- Right lower quadrant tenderness
- Signs of localized or generalized peritoneal irritation such as:
- Involuntary muscle guarding with abdominal palpation
- Positive Rovsing sign (pain in the right lower quadrant with palpation of the left side)
- Obturator sign (pain on flexion and internal rotation of the right hip, which is seen when the inflamed appendix lies in the pelvis and causes irritation of the obturator internus muscle)
- Iliopsoas sign (pain on extension of the right hip, which is found in retrocecal appendicitis)
- Rebound tenderness (elicited by the examiner placing steady pressure with his or her hand in the right lower quadrant for 10 to 15 seconds and then suddenly releasing the pressure; a positive finding consists of increased pain with removal of pressure)
*** The practitioner must have a high index of suspicion in this age group; as appendicitis is rare, and symptoms may not be typical, children under 5 are at greatest risk for delay in diagnosis with subsequent perforation
● White blood cell count (WBC)
● Differential with calculation of the absolute neutrophil count (ANC)
● C-reactive protein (CRP)
● Urinalysis
WBC Count: Either the WBC or the ANC is elevated in up to 96 percent of children with appendicitis
CRP: Elevation of CRP has been associated with appendicitis, however sensitivities and specificities vary. CRP appears to be less sensitive in patients who have had symptoms for less than 24 hours but more sensitive than WBC for patients with symptoms for 24 to 48 hours.
The Pediatric Appendicitis Score
[table class=”table-striped”]
Item,Score (Point)
Anorexia,1
Nausea or vomiting,1
Migration of pain,1
Fever >38°C (100.5°F),1
Pain with cough\, percussion or hopping,2
Right lower quadrant tenderness,2
White blood cell count >10\,000 cells/microL,1
Neutrophils plus band forms >7500 cells/microL,1
Total,10 Points
[/table]
C: Centigrade; F: Fahrenheit.
● A PAS ≤2 or 3 suggests a low risk for appendicitis. Children with a PAS score in this range may be discharged home as long as their caretakers understand that persistent pain or additional symptoms warrant repeat evaluation.
● A PAS ≥7 or 8 indicates a high risk for appendicitis. Children with a PAS score in this range warrant surgical consultation or urgent imaging depending upon local guidelines. It is unclear if the PAS alone can be used to determine the need for appendectomy, because the number of patients with high scores who do not have appendicitis varies widely.
● A PAS of 3 to 6 or 7 is indeterminate for appendicitis. The best approach is not clear. Options include surgical consultation, diagnostic imaging, serial abdominal examinations while being observed in the hospital, or a combination of these approaches depending upon local resources.
The frequency of appendicitis in several studies varies by PAS as follows:
●PAS ≤2 to 3 – 0 to 2 percent
●PAS 3 to 6 – 8 to 48 percent
●PAS ≥7 – 78 to 96 percent
Diagnostic approach to pediatric appendicitis
2. Bundy DG, Byerley JS, Liles EA, et al. Does this child have appendicitis? JAMA 2007; 298:438.
3. Scholer SJ, Pituch K, Orr DP, Dittus RS. Clinical outcomes of children with acute abdominal pain. Pediatrics 1996; 98:680.
4. Colvin JM, Bachur R, Kharbanda A. The presentation of appendicitis in preadolescent children. Pediatr Emerg Care 2007; 23:849.
Neurology
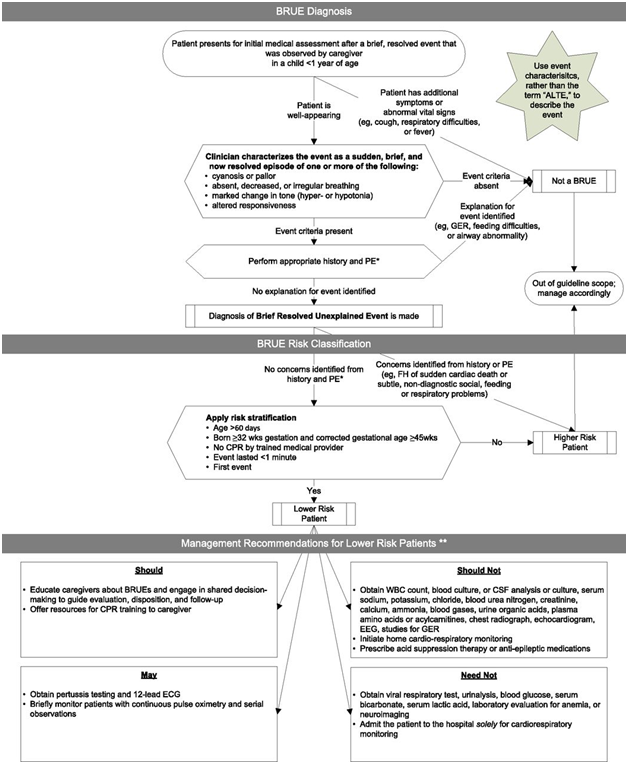
BRUE Clinical Practice Guidelines
New Clinical Practice Guideline published by the AAP, has 3 main objectives:
1) Recommends the replacement of the term ALTE with a new term, brief resolved unexplained event (BRUE).
2) Provides an approach to patient evaluation that is based on the risk that the infant will have a repeat event or has a serious underlying disorder.
3) Provides management recommendations, or key action statements, for lower-risk infants.
Thus, the development of a definition (BRUE) that allows a direct sequence to base clinical decisions upon; events that are characterized as abnormal after conducting a thorough history and physical examination.
(1) cyanosis or pallor
(2) absent, decreased, or irregular breathing
(3) marked change in tone (hyper- or hypotonia)
(4) altered level of responsiveness
***Clinicians should diagnose a BRUE only when there is no explanation for a qualifying event after conducting an appropriate history and physical examination. Ie: Diagnosis of BRUE excludes the presence of fever, respiratory symptoms, vomiting, bruising, etc.
Recommendations provided for BRUE apply only to “low-risk” infants, who are defined by:
(1) age >60 days
(2) gestational age ≥32 weeks and postconceptional age ≥45 weeks
(3) occurrence of only 1 BRUE (no prior BRUE ever and not occurring in clusters)
(4) duration of BRUE (5) no cardiopulmonary resuscitation by trained medical provider required
(6) no concerning historical features
(7) no concerning physical examination finding
***Infants who have experienced a BRUE who do not qualify as lower risk patients are, by definition, at higher risk. No recommendations for infants considered “high risk” are provided.
Management of BRUE
In the absence of identifiable risk factors, laboratory studies, imaging studies, and other diagnostic procedures are unlikely to be useful or necessary in infants considered “low risk”.
The ALTE literature supports that infants presenting with a lower-risk BRUE do not have an increased rate of cardiovascular or other events during admission and hospitalization may not be required, but close follow-up is recommended.
Pediatric Head CT Algorithm
[table]
Age,Symptom,Treatment
< 2 yr [attr rowspan=2],GCS = 14 or signs of altered mental status, CT Head
GCS = 15 but “not acting like self”
History of LOC > 5 sec
Scalp hematoma
Severe mechanism of injury, Observer vs Head CT
>2 yr [attr rowspan=”2″],GCS=14 or AMS or basilar skull fracture,CT Head
History of LOC\, vomiting\, headache\, OR severe mechanism of injury,Observe vs Head CT
[/table]
Seizures (Status Epilepticus)
0-5 minutes:
– ABCDE, oxygen, monitors
– IV access, glucose check
– Brief H&P
– Initial Labs: CBC, CMP, Mg, Phos, HCG, Tox, Med levels
5-10 minutes:
– IF IV ACCESS OBTAINED: Lorazepam (Ativan) 0.1mg/kg IV (max 4mg)
– IF NO IV ACCESS: Midazolam (Versed) 0.3mg/kg Buccal/IM/IN (max 10mg)
or Diazepam (Valium) 0.5mg/kg Rectal (max 20mg)
– second dose of Lorazepam 0.1mg/kg IV (max 4mg)
10-20 minutes:
**SECOND MEDICATION:
-Levetiracetam (Keppra) 50mg/kg IV (max 2500mg)
or Fosphenytoin 20mg/kg IV
20-40 minutes:
**THIRD MEDICATION:
-Fosphenytoin 20mg/kg IV
or Valproate 40mg/kg IV
or Levetiracetam 50mg/kg
-Notify PICU and Neurology (4th Medication Recommendations)
**SECOND/THIRD MEDICATION CHOICE:
-If on Levetiracetam <80mg>80mg/kg/day:
2nd med Fosphenytoin, 3rd med Valproate
– If on Phenytoin:
2nd med Levetiracetam, 3rd med Valproate
*If patient received a benzo dose prior to arrival, consider advancing to a 2nd agent after the first lorazepam dose
Source: http://www.chop.edu/clinical-pathway/status-epilepticus-clinical-pathway (accessed 6/27/16)
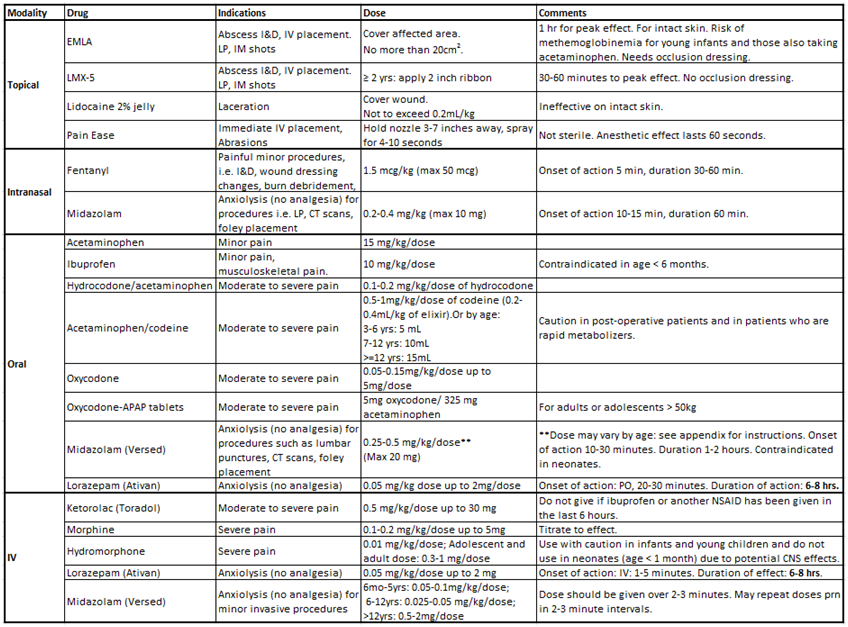
Pain Management
Pain-free ED Initiatives for Pediatric ED
Goal: To improve pain control and decrease anxiety for our patients in the pediatric emergency department during minor painful or stressful procedures.
Note: This protocol is not meant to address procedural sedation.
For painful procedures:
1. Topical anesthetics should be applied in anticipation of a painful procedure, as appropriate (see below).
2. Systemic (oral, intranasal, or parenteral) analgesia and/or anxiolysis should be provided prior to the painful procedure as appropriate (see below).
3. During the procedure:
- One dedicated person (Registered Nurse (RN), Multifunction Technician, Child Life), if available, to provide procedural support to child: distraction (toys, books, music, bubbles), relaxation (guided imagery, positive touch).
- Encourage parent interaction (if appropriate).
4. After the procedure: Help child regroup, calm, recover.
**Please note that EMLA, LMX-5, LET, Pain Ease, Sweet Ease, and Acetaminophen and Ibuprofen are part of nurses’ advanced treatment protocols, and can be administered by the RN according to the protocol.**
A. Topical anesthetics (See Appendix A):
Triage RN, RN Responsibilities:
Prior to an anticipated painful procedure, the RN should place a topical anesthetic: LET prior to laceration repair, EMLA or LMX-5 prior to IV placement if time permits or prior to incision and drainage of an abscess, Pain Ease prior to IV catheter placement or venipuncture if there is not enough time for placement of EMLA or LMX-5.
Physician, Physician Assistant (PA) Responsibilities:
If a topical anesthetic has not already been placed by RN in advanced triage, the physician or PA will consider topical anesthetic prior to a painful procedure: LET prior to laceration repair, EMLA or LMX-5 prior to incision and drainage of an abscess, Pain Ease prior to IV catheter placement or venipuncture if the IV catheter is needed quickly.
[table class=”table-striped table-col-border”]
In anticipation of:,EMLA,LMX-5,LET,Pain Ease
IV placement / venipuncture, ✔ (if time permits)[attr colspan=”2″],,✔
Laceration Repair,,,✔,
Abscess (I & D),✔,✔,,
Lumbar puncture, IM shots, arterial puncture,✔,✔
Abrasion,,,✔,✔
Onset to peak effect:,60 min.,30 – 60 min.,30-60 min.,immed.
Notes,, Use for ≥ 2 yrs of age,,Not Sterile
[/table]
B. Non-pharmacologic approaches for a patient in acute pain or with high levels of anxiety:
- Behavioral distraction (age-appropriate toys in our age-based procedural pain kits, iPad applications).
- Cognitive strategies (breathing exercises, relaxation training).
- Physical strategies (comfort positioning, heat/cold therapy, massage).
C. Sweet Ease for neonates/infants (See Appendix A)
D. Pharmacologic agents for acute pain: (See Appendix A)
1. Oral analgesics
RN Responsibilities:
- For mild pain, the RN should administer Acetaminophen 15 mg/kg/dose PO/PR every 4 hours as needed for mild pain or Ibuprofen 10 mg/kg/dose PO every 6 hours as needed for pain.
- Ibuprofen is preferred for musculoskeletal pain.
- Ibuprofen is contraindicated for use in patients < 6 months old.
PA/Physician Responsibilities:
Note: PA’s are encouraged to follow the same protocol, and the attending physician should be made aware when giving non-topical pharmacologic analgesics.
For moderate to severe pain, the following oral narcotics are available in the Pyxis:
Hydrocodone/Acetaminophen
- 1-0.2 mg/kg/dose of hydrocodone (0.2-0.4 mL/kg of elixir) PO every 4 hours prn moderate to severe pain.
- Available as hydrocodone 7.5mg/ acetaminophen 500mg per 5mL liquid.
Oxycodone
- 05-0.15 mg/kg/dose every 4 hours prn moderate to severe pain.
- Maximum dose: 5mg/dose.
- Available as oxycodone 5mg/5mL oral solution or as a 5 mg immediate release tablet.
Oxycodone-APAP
- For adolescent/adult or >50 kg: One (1) tablet every 4 hours prn moderate to severe pain.
- Available as oxycodone 5mg / acetaminophen 325 mg tablets.
Acetaminophen/codeine
- 5-1 mg/kg/dose of codeine (0.2-0.4 mL/kg of elixir) PO every 4 hours prn moderate to severe pain.
- Available as codeine 12 mg and acetaminophen 120 mg per 5 mL oral solution, or as 30 mg tablets.
- Can also be dosed by age:
- 3-6 years: 5 mL (12 mg codeine + 120 mg acetaminophen) PO every 6 hours prn moderate to severe pain.
- 7-12 years: 10 mL (24 mg codeine + 240 mg acetaminophen) PO every 6 hours prn moderate to severe pain.
- ≥12 years: 15 mL (36 mg codeine + 360 mg acetaminophen) PO every 4 hours prn moderate to severe pain.
- Caution:
- Life-threatening adverse events and death have occurred in certain children who received codeine after tonsillectomy and/or adenoidectomy for obstructive sleep apnea syndrome. These children had evidence of being “ultra-rapid metabolizers” of substrates of cytochrome P450 2D6, including codeine.
- If prescribing codeine-containing drugs, use the lowest effective dose for the shortest period of time on an as-needed basis (i.e., not scheduled around the clock).
- Do not use in children < 3 years old.
2. Intranasal fentanyl (See Appendix A):
Intranasal fentanyl is available as a needleless analgesic that can be delivered via the mucosal atomization device (MAD).
- The starting dose is 1.5 mcg/kg (max 50 mcg).
- Onset of action: 5 minutes. Duration: 30-60 minutes.
- As with all opiates, may need to titrate to effect.
- When ordering intranasal medications, the licensed independent provider must write out the word “intranasal” and cannot abbreviate “IN” to avoid any medication errors.
Examples of painful procedures for which intranasal fentanyl would be appropriate: incision and drainage, wound-dressing/ packing changes, laceration repair, burn debridement/dressings, other minor procedures.
3. Parenteral analgesics [Intravenous (IV), Intramuscular (IM)]:
Ketorolac (Toradol)
- 5 mg/kg/dose up to 30 mg IV every 6 hours prn moderate to severe pain.
- Approved for age >2 years old.
- **Do not give if ibuprofen or another NSAID has been given in the last 6 hours**
Morphine
- 1-0.2 mg/kg/dose every 3 hours prn severe pain.
- Adolescent and adult standard starting dose: 2-5 mg/dose every 2-6 hours prn severe pain.
- May give higher doses in patients with developed tolerance from long-term use.
- Titrate to effect.
Hydromorphone
- 01 mg/kg/dose every 4 hours prn severe pain.
- Adolescent and adult dose: 0.3-1 mg/dose every 4-6 hours prn severe pain.
- **Use with caution in infants and young children and do not use in neonates (age < 1 month) due to potential CNS effects.**
E. Pharmacologic agents for anxiolysis: (See Appendix A)
PA/Physician Responsibilities:
**Intent is anxiolysis with maintenance of consciousness. Obtained when a single drug is given at a low to moderate dose. If more than one agent is given (i.e. benzodiazepine and a narcotic) then this is considered moderate sedation, and the procedural sedation guidelines for monitoring should be followed.**
Indications: Consider using an agent for anxiolysis for procedures such as: lumbar puncture, CT scan for young/anxious children, foley catheter placement, foreign body removal, pelvic exam.
1. Oral agents for anxiolysis:
Lorazepam (Ativan). Standard dose for anxiolysis: 0.05 mg/kg dose every 4-8 hours PO, maximum dose: 2 mg/dose. Onset of action: 20-30 minutes. Duration of action: 6-8 hrs.
Midazolam (Versed). Standard dose for age >6 months: 0.25-0.5 mg/kg/dose PO x1, maximum dose: 20 mg. Onset of action: 10-30 min; Duration: 1-2 hours.
- Younger patients (6 months – 5 years) may require higher total doses of 1mg/kg/dose, whereas older patients (6-15 yrs) may require only 0.25 mg/kg/dose. Use 0.25 mg/kg/dose for patients with cardiac or respiratory compromise, concurrent CNS depressive drug, or high-risk surgery.
- Use lower doses when given in combination with narcotics.
- Has rapid and predictable onset of action, a short recovery time. Causes amnesia. Results in mild depression of hypoxic ventilatory drive.
- Contraindicated in neonates (age < 1 month).
- Causes respiratory depression, hypotension, and bradycardia.
2. Intranasal midazolam for anxiolysis:
- The dose of intranasal midazolam is 0.2-0.4mg/kg (max 10 mg) to be given via the mucosal atomization device (MAD).
- Onset of action is 10-15 minutes. Duration is 60 minutes.
- Nasal burning may occur with intranasal midazolam and may last 30 seconds.
- When ordering intranasal medications, the licensed independent provider must write out the word “intranasal” and cannot abbreviate “IN” to avoid any medication errors.
3. Parenteral (IV/IM) agents for anxiolysis
IV Lorazepam (Ativan).
- Dose: 0.05 mg/kg/dose every 4-8 hrs, max dose 2 mg/dose.
- May also be given IM at same dose.
- Onset of action: IV: 1-5 minutes, IM, 30-60 minutes. Duration: 6-8 hrs.
IV Midazolam (Versed)
- Standard dose:
- For ages 6 months to 5 yrs is 0.05-0.1 mg/kg/dose; initial dose up to 2 mg, with a max total dose of 6 mg. A total dose up to 0.6 mg/kg may be necessary for desired effect.
- For ages 6-12 yrs, standard dose is 0.025-0.05 mg/kg/dose. Initial dose up to 2 mg, with a max total dose of 10 mg. A total dose up to 0.4 mg/kg may be necessary for desired effect.
- For adolescents >12 yrs, use adult dose of 0.5-2 mg/dose. Usual total dose 2.5-5 mg; max total dose 10 mg.
- Dose should be given over 2-3 minutes.
- May repeat doses prn in 2-3 minute intervals.
Monitoring
- Cardiorespiratory monitoring should be used when a single IV or intranasal agent (i.e. either a benzodiazepine or a narcotic) is being used.
- If multiple agents are being used (i.e. a benzodiazepine in combination with a narcotic), then this is considered moderate sedation, and the procedural sedation guidelines for monitoring should be followed.
Rectal midazolam dose from: Saint-Maurice C, Meistelman C, Rey E et al: The pharmacokinetics of rectal midazolam for premedication in children. Anesthesiology 65:536, 1986
Intranasal fentanyl dose from various concordant sources including: Borland M, Jacobs I, King B, O’Brien D. A randomized controlled trial comparing intranasal fentanyl to intravenous morphine for managing acute pain in children in the emergency department. Ann Emerg Med. 2007;49(3):335–340
Intranasal midazolam dose from various concordant sources including: Lane RD, Schunk JE. Atomized intranasal midazolam use for minor procedures in the pediatric emergencydepartment. Pediatr Emerg Care. 2008;24(5):300–303
Appendix A – Topical and intranasal agents in the pediatric ED: Instructions for use
A. Sweet Ease (sucrose 24%)
- Administer 0.2-0.5 mL (equivalent to 1-2 drops or 1 pacifier dip) of Sweet Ease by mouth via pacifier.
- May repeat every 30 seconds for a maximum of 2 minutes.
- Indications: procedures such as heel sticks, immunizations, venipuncture, IV line insertion, arterial puncture, insertion of a foley catheter and lumbar puncture in neonates and infants.
- Age: Strongest evidence for infants 0-1 month but some studies show efficacy up to 12 months.
B. Topical
- Indications: Incision and drainage of abscess, peripheral IV catheter insertion, venipuncture, lumbar punctures, arterial sticks, port access, or PICC line insertions.
- Dose:
- For infants <3 kg:
- Maximum application area of 10cm2 (diameter 1.5 inches) and maximum application time is 1 hour.
- For children 3-20 kg:
- Maximum application area of 20cm2 (diameter of 2 inches).
- For adults and children > 20 kg.
- Maximum application area of 25 cm2 (diameter of 2.5 inches).
- For infants <3 kg:
- Instructions for use:
- EMLA is intended for use on normal intact skin; avoid contact near eyes, on open wounds, or on mucous membranes. The rationale for this is related to the risk of acquired methemoglobinemia. However, a few recent studies have used EMLA on minor open wounds safely and efficaciously without reported complications. EMLA may be used on minor open wounds at the physician’s discretion.
- Cover the EMLA cream so that you get a thick layer underneath. Do not spread out the cream.
- EMLA should be applied at least one hour before the start of a painful procedure (such as intravenous cannulation, venipuncture, IM injections, lumbar puncture)
- Leave on for 60 minutes for best anesthetic effect. However, the anesthetic effect exists on a continuum and studies have shown decrease in pain starting 30 minutes after application.
- Remove the occlusive dressing, wipe off the EMLA cream, clean the entire area with an antiseptic solution and prepare the patient for the procedure. The duration of effective skin anesthesia will be at least one hour after removal of the occlusive dressing.
- CAUTIONS/CONTRAINDICATIONS:
- Due to the risk of acquired methemoglobinemia from systemically absorbed prilocaine, EMLA should be avoided in patients:
- with history of methemoglobinemia
- under 1 year old AND taking any of the following medications: acetaminophen, class I antiarrhythmics, chloroquine, nitrates, dapsone, nitrofurantoin, phenobarbital, phenytoins, primaquine, sulfonamides
- taking any class III antiarrhythmic drugs (amiodarone, dofetilide, ibutilide, sotalol)
- and should be used with caution in patients with history of:
- hepatic disease
- G6PD deficiency
- sepsis
- severe shock
- heart block
- or in patients taking any of the following medications: acetaminophen, class I antiarrhythmics, chloroquine, nitrates, dapsone, nitrofurantoin, phenobarbital, phenytoins, primaquine, sulfonamides
- Due to the risk of acquired methemoglobinemia from systemically absorbed prilocaine, EMLA should be avoided in patients:
- Indications: venipuncture, peripheral IV catheter insertion, IM injections. May also consider for incision and drainage of small abscesses, foreign body removal, suture removal.
- Dose: For ≥ 2 years of age: Apply 2-inch ribbon.
- Instructions for use:
- Clean injection site.
- Apply age-specific amount to the affected area. Gently rub the medicine in until it is evenly distributed.
- No occlusion dressing is required (but may be occluded to prevent disturbance).
- Anesthetic effect starts within 30 minutes and lasts approximately 60 minutes after wiping the cream off.
- Wipe area clean with gauze swab 5 minutes prior to procedure. Maximum application time is 60 minutes.
- Note: although the product is labeled “for anorectal pain”, it can be used on normal skin at any site.
- CAUTIONS/CONTRAINDICATIONS:
- Use with caution in patients with epilepsy, severe hepatic disease, severe renal impairment, sepsis, or shock.
- Use with caution in patients also taking class I antiarrhythmics (tocainide, mexiletine) or class III antiarrhythmics (amiodarone).
- Indications: Open wounds, laceration repair
- Dose: Not to exceed 4.5 mg/kg (0.22 mL/kg) of the jelly. When using both topical and injected lidocaine or lidocaine with epinephrine, the provider should take both topical and injected lidocaine into consideration when considering maximum total doses (Refer to Harriet Lane Handbook).
- Instructions for use: Apply a moderate amount of jelly to the surface of the wound. No occlusion dressing is required (but may be occluded to prevent disturbance). Onset of action is 5 minutes. It is ineffective when applied to intact skin
- Indications: Peripheral IV catheter insertion, venipuncture, injections. Also consider for incision and drainage of small abscesses, foreign body removal, suture removal, pre-lidocaine injections (i.e. for laceration repair), and for abrasions.
- Instructions for use:
- Clean injection site.
- Hold nozzle 3-7 inches from target. Spray steadily onto the site for 4-10 seconds. As soon as the skin starts to turn white, stop.
- Anesthetic effect lasts approx 60 seconds. Reapply as needed.
- Note: this is not a sterile item. Do not use when drawing blood cultures.
C. Intranasal agents
- Indications: For analgesia for orthopedic injuries/minor fractures, and painful procedures such as:
- incision and drainage
- wound-dressing/ packing changes
- laceration repair
- burn debridement/dressings
- other minor procedures
- Dose: The starting dose is 1.5 mcg/kg. (maximum: 50mcg). As with all opiates, may need to titrate to effect. Onset of action: 5 minutes. Duration: 30-60 minutes.
- Instructions:
- Administer half of total dose per nostril (If order is written for “fentanyl 100mcg intranasally x1 now”, administer 50 mcg of fentanyl in each nostril).
- For ideal effect and absorption, no more than 1.0mL should be given per nostril. Limiting the dose to even smaller amount, such as 0.5mL, may improve absorption and reduce runoff.
- If a higher dose is needed, it should be given in several doses a few minutes apart.
- To maximize clinical effectiveness, the intranasal dose should be administered using the mucosal atomization device (MAD).
- Large amounts of mucus or blood will inhibit medication absorption.
- The medication can be administered by a nurse or a doctor.
- When using the MAD the dose should be given quickly to ensure atomization of the particles.
- For administration, use the syringes with approved labels: “NOT FOR IV USE”.
- Dose: 0.2-0.4 mg/kg (max 10 mg). Onset of action is 10-15 minutes. Duration is 60 minutes.
- Indications: For anxiolysis for procedures such as:
- laceration repair
- lumbar puncture
- CT scan for young/anxious children
- IV insertion/ venipuncture
- foley catheter placement
- foreign body removal
- Instructions:
- Administer half of total dose per nostril (If order is written for “Versed 10 mg intranasally x1 now”, administer 5 mg of Versed in each nostril).
- For ideal effect and absorption, no more than 1.0mL should be given per nostril. Limiting the dose to even smaller amount, such as 0.5mL, may improve absorption and reduce runoff.
- If a higher dose is needed, it should be given in several doses a few minutes apart.
- To maximize clinical effectiveness, the intranasal dose should be administered using the mucosal atomization device (MAD).
- Large amounts of mucus or blood will inhibit medication absorption.
- The medication can be administered by a nurse or a doctor.
- When using the MAD, the dose should be given quickly to ensure atomization of the particles.
- For administration, use the syringes with approved labels: “NOT FOR IV USE”.
- Nasal burning may occur with intranasal midazolam and may last 30 seconds.
Appendix B: Quick Reference
Respiratory
Bronchiolitis
The following set of guidelines applies for children 1 to 23 months of age.
The most common etiology of bronchiolitis is respiratory syncytial virus (RSV), with the highest incidence of infection occurring between December and March in North America. Infection with RSV does not grant permanent or long-term immunity, with reinfections common.
Other viruses that cause bronchiolitis include human rhinovirus, human metapneumovirus, influenza, adenovirus, coronavirus, human, and parainfluenza viruses.
Important issues to assess in the history include the effects of respiratory symptoms on mental status, feeding, and hydration. The clinician should assess the ability of the family to care for the child and to return for further evaluation if needed.
History of underlying conditions, such as prematurity ,cardiac disease, chronic pulmonary disease, immunodeficiency, or episodes of previous wheezing, should be identified; as these are risk factors for severe disease.
Tobacco smoke use – tobacco smoke exposure increases both severity of illness and risk of hospitalization for bronchiolitis. Studies have shown there is evidence that counseling parents in these settings is well received and has a measurable impact on disease course.
Chest x-ray: Should be reserved for severe cases only – ie: those severe enough to warrant ICU admission or where signs of an airway complication are present. Otherwise, xray use often leads to unnecessary antibiotic use, with no particular change in outcome.
Nebulized Epinephrine: not recommended for use in bronchiolitis secondary to a lack of efficacy compared with placebo, except potentially as a rescue agent in severe disease.
Nebulized Hypertonic Saline: not recommended for use in bronchiolitis in the outpatient or emergency department setting. Studies show it does not decrease LOS in settings where expected stays are less than 3 days; trials have shown some reduction in LOS for those in which the duration exceeds 3 days.
Corticosteroids: not recommended for use in bronchiolitis in any setting. Use does not significantly reduce outpatient admissions or length of stay, and may actually prolong viral shedding in patients with bronchiolitis.
Oxygen Saturation: Oxygen saturation of 90% or above should be tolerated in infants and children with bronchiolitis, as no data exist to suggest such increases beyond 90% result in any clinically significant difference in physiologic function, patient symptoms, or clinical outcomes.
Chest Physiotherapy: not recommended, as no clinical benefit has been found by using vibration or percussion, or passive expiratory techniques. Deep suctioning is also not recommended, as it has been associated with a longer LOS in hospitalized infants 2 to 12 months of age.
However, external, noninvasive suctioning IS recommended, as studies have shown that lapses of greater than 4 hours in noninvasive, external nasal suctioning are associated with longer LOS.
Antibacterials: not recommended in bronchiolitis, as no benefit from use has been shown. Studies have shown that febrile infants without an identifiable source of fever have a risk of bacteremia that may be as high as 7%. However, a child with a distinct viral syndrome, such as bronchiolitis, has a lower risk (much less than 1%) of bacterial infection of the cerebrospinal fluid or blood.
Nutrition and Hydration: Clinicians should administer nasogastric or intravenous fluids for infants with a diagnosis of bronchiolitis who cannot maintain hydration orally; this accounts for approximately one third of hospitalized cases. No significant or statistical difference has been measured between use of formula via NG tube or dextrose containing IV fluids.
HAND HYGEINE – RSV can remain infectious on counter tops for ≥6 hours, on gowns or paper tissues for 20 to 30 minutes, and on skin for up to 20 minutes.
Hands should be disinfected before and after direct contact with every patient, after contact with inanimate objects in the direct vicinity of the patient, and before putting on and after removing gloves. If hands are not visibly soiled, an alcohol-based rub is preferred. Use of PPE is also preferred.
Use of palivizumab – see recommendations for age and disease history
Online version of this article available at: http://pediatrics.aappublications.org/content/early/2014/10/21/peds.2014-2742
Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and Management of Bronchiolitis. Pediatrics. The Official Journal of the American Academy of Pediatrics. 01 October 2006. Vol 188. No 4. Pages 1774 – 1793.
Online version of this article available at:
http://pediatrics.aappublications.org/content/118/4/1774.full
Croup
Croup (laryngotracheitis) is a common illness responsible for up to 15 percent of emergency department visits due to respiratory disease in children in the United States.
Croup symptoms usually start like an upper respiratory tract infection, with low-grade fever and coryza followed by a barking cough and various degrees of respiratory distress. In most children, the symptoms subside quickly with resolution of the cough within two days.
Etiology
Croup is usually caused by viruses, which are detected in up to 80 percent of patients. The most common cause is parainfluenza virus. The table below displays the most common viruses associated with croup, as well as their frequency, severity, and peak time of presentation.
[table class=”table-striped”]
Etiology,Frequency,Severity,Peak Incidence
Parainfluenza virus types 1 to 3 (type 1 is most common),Frequent,Variable (usually severe with type 3 virus),Winter and spring
Enterovirus,Occasional to frequent,Usually mild,Fall
Human bocavirus,Occasional to frequent,Usually mild,Spring and fall
Influenza A and B viruses,Occasional to frequent,Variable (severe with influenza A virus),Winter
Respiratory syncytial virus,Occasional to frequent,Mild to moderate,Winter
Rhinovirus,Occasional to frequent,Usually mild,Fall
Adenovirus,Occasional,Mild to moderate,Winter
[/table]
Pediatric RSI Guidelines 2016
Step 1 – Prepare
Equipment, personnel, monitors,
Prepare for difficult airway( video assist, LMA available)
Step 2 – Preoxygenate/100%
FiO2 via 100% nonreabreather for 2-3 min. Avoid positive pressure bag-valve-mask unless necessary. Consider additional oxygen via nasal cannula during intubation @ 15L/min HFNC or 5L/min.
Step 3– Premedication/Prevention (each as indicated).
Adequate volume resuscitation
Vagolytics – Atropine consider for all children < 1 year (laryngoscopy induced bradycardia), children <5 receiving first dose of succinylcholine, older children receiving second dose of succinycholine, patients experiencing bradycardia prior to intubation
ICP Protection -Lidocaine
Analgesia (only if indicated. Can be used for pain and sedation. Not first choice)
Step 4 – Sedate (choose 1)
Normotensive
Propofol, Etomidate
Hypotensive
Ketamine, Etomidate
Avoid: propofol, versed (↓BP)
Septic Shock
Ketamine.
Caution: Etomidate(adrenal suppression) propofol(↓BP), versed (↓BP)
Status Asthmaticus
Ketamine, etomidate
Status Epilepticus
Propofol, midazolam
Caution: Etomidate
Head Injury/Increased ICP
Etomidate (unless sz), propofol
Caution: Ketamine
Step 5 – Cricoid Pressure
Optional step. No proven benefit in preventing gastric aspiration.
Step 6 – Neuromuscular Blockade (choose 1)
None – may consider no neuromuscular blockade in first attempt with anticipated difficult airway
Succinycholine – IDEAL AGENT unless contraindications. Rapid acting and short duration.
Rocuronium – CAUTION w difficult airway or inexperience 2/2 long duration
Step 7 – Tracheal Intubation after full muscle relaxation with confirmation
Clinical and
ETCO2 and
pulsox and
CXR – ideal=2cm above carina
(ETCO2 either capnogrophy or colorimetric CO2 detector; use peds device <15 kg, use adult device> 15kg: not accurate if low pulm blood flow (ie cardiac arrest)
Step 8
Place NG or OG if not done already
Step 9 – Post-intubation monitoring
continuous pulsox
continuous capnography
mechanical ventilation
ABG
Step 10 – Continued analgesia and sedation
Sedation (and analgesia if needed)
Propofol infusion, diazepam, fentanyl
If long acting paralytics are needed
Vecuronium, pancuronium Avoid: Succinycholine
[table class=”table-striped”]
Drug,Induction Dose,Time of Onset,Duration ,Comment
Premedications (when needed)[attr colspan=”5″ style=”background:#ccc”]
Atropine, 0.01-0.02mg/kg IV\, max 0.5mg (can be given IM 0.02mg/kg), Within seconds,>30 minutes,Give 1-2 minutes prior to any sedative or paralytic
Lidocaine,1-2mg/kgIV,1-3 minutes,30 minutes,Give 2-5 minutes prior to intubation to pts with ↑ ICP
Sedatives [attr colspan=”5″ style=”background:#ccc”]
Etomidate,0.2-0.4 mg/kg IV,Within seconds,10-15 minutes,Favorable side effect profile; min CV effects. decreases ICP/IOP; may cause myoclonus Avoid in suspected septic shock (adrenal suppression). ↓ seizure threshold in pts with known seizure d/o
Ketamine,1-3mg IV (Can be given IM 2-4mg/kg),1-2 minutes,10-15 minutes,Preserves airway reflexes and resp drive; bronchodilator; + analgesia
Caution in ICP and ocular pressure and HTN (evidence not strong); increases secretions; rare instances of laryngospasm
Propofol,1-2 mg/kg IV bolus (up to 3mg/kg/min in age 6 mos-5 years),Within seconds,10-15 minutes,Neuroprotective effect. Suppresses seizure activity.
Significant myocardial depressant; ↓BP; ↓resp drive; met acidosis;
Consider other options in patients with hx anaphylaxis to egg/soy
Versed,0.1-0.3mg/kg IV max single dose 10mg, 2-5 min,15-30 minutes,Anticonvulsant properties Consider more favorable agents first Respiratory depression\, myocardial depression\, ↓BP. Avoid in hemodynamically unstable patients.
Neuromuscular blockade [attr colspan=”5″ style=”background:#ccc”]
Succinycholine,1-2 mg IV (Can be given IM 4mg/kg), 20-60 seconds, 4-6 minutes, Most widely used 2/2 short brief Duration
Bradycardia especially with repeated doses(extreme cases asystole) –atropine premedication in patients < 5years; transient muscle fasciculations\, which may be important in pts with ↑ICP or ↑ocular pressure\, transient ↑K+ in healthy patients; potentially life-threatening ↑K+ in at-risk patients
Strictly Avoid: pre-existing hyperkalemia\, crush injury\, multsytem trauma\, burns >48hr\, denervating neurologic disorders; skeletal myopathies; malignant hyperthermia
Do not use for maintenance paralysis
Caution: Increased ICP or IOP
Rocuronium, 0.6mg-0.9mg/kg, 30-60 seconds, 30-60 minutes, Long duration = caution with difficult airway or inexperience.
Succinycholine is usually better choice. Rarely ↑HR\, ↑BP
Post Intubation [attr colspan=”5″ style=”background:#666;color:white”]
Sedatives (post intubation) [attr colspan=”5″ style=”background:#ccc”]
Propofol,Continuous sedation
10-240 micrograms/kg/min (0.6 – 15mg/kg/hour),,,Neuroprotective effect. Suppresses seizure activity.
Significant myocardial depressant; ↓BP; ↓resp drive; met acidosis;
Consider other options in patients with hx anaphylaxis to egg/soy
Fentanyl,1-3mcg/kg IV,1-2 minutes,30-40 minutes,May cause chest wall rigidity; may also cause ↑ ICP; may ↓BP. Consider safer more effective options for sedation.
Diazepam, 0.1-0.2 mg/kg max 4mg, 2-3 minutes, 30-90 minutes,
Paralytics (post intubation) [attr colspan=”5″ style=”background:#ccc”]
Vecuronium,0.1-0.3mg/kg IV,2-5 min,30-60 minutes,Primarily used for maintenance paralysis
Pancuronium,0.1mg/kg,1-5min,120-150 min,Primarily used for maintenance paralysis
[/table]
2. Staple, L, O’Connell,K. Pediatric Rapid Sequence Intubation. Pediatric Trauma Care 11/@2014 AHC Media LLC.
3. Weingart, S, Levitan, R. Preoxygenation and Prevention of Desaturation During Emergency Airway Management. Annals of Emergency Medicine. 2012;59:165-175.
4. PALS – AHA 2015
5. 2016 eBroselow
Respiratory Synctial Virus (RSV)
RSV is the most common cause of lower respiratory tract infection (LRTI) in children younger than one year. Globally, it is estimated that RSV causes about 34 million episodes of acute lower respiratory infections in children younger than five years, resulting in about 3.4 million hospitalizations per year.
RSV commonly causes lower respiratory tract infection; most commonly bronchiolitis. Bronchiolitis is characterized by acute inflammation, edema, and necrosis of epithelial cells lining small airways, and increased mucus production. Infection with RSV does not grant permanent or long-term immunity, with reinfections common.
Important issues to assess in the history include the effects of respiratory symptoms on mental status, feeding, and hydration. The clinician should assess the ability of the family to care for the child and to return for further evaluation if needed.
History of underlying conditions, such as prematurity ,cardiac disease, chronic pulmonary disease, immunodeficiency, or episodes of previous wheezing, should be identified; as these are risk factors for severe disease.
Emergency room management & inpatient admission should be considered in a patient that presents with one or more of the following: hypoxia, increased work of breathing, decreased oral intake, or history of one of the above listed risk factors.
Risk of Apnea – studies show that the following risk factors increase the risk for apnea – age less than one month (with immediate inpatient admission recommended for <2 weeks of age), age < 37 weeks gestation at birth, history of witnessed apneic event prior to ED arrival, and oxygen saturation <92% upon ED arrival. Therefore, it is recommended that anyone < 2 weeks of age, and/or with history of home event, and/or with low oxygen saturation at presentation should be kept for observation at a minimum. The majority of apneic events have been shown to occur within 48 hours of hospitalization. Age > 6 months confers very low risk for predicted apneic event to occur.
In general practice, both clinicians and families are eager to know whether the etiologic agent is RSV, or one of its counter viruses. However, it is not cost or time effective to test everyone. Therefore, if testing will make a change in clinical status – ie: hospitalization vs discharge, hospital placement, risk of exposure to others, etc. then only should routine testing take place.
Chest x-ray: Should be reserved for severe cases only – ie: those severe enough to warrant ICU admission or where signs of an airway complication are present. Otherwise, xray use often leads to unnecessary antibiotic use, with no particular change in outcome.
Nebulized Epinephrine: not recommended for use in bronchiolitis secondary to a lack of efficacy compared with placebo, except potentially as a rescue agent in severe disease.
However, often in practice children have shown to be responsive to one of the above treatments. Therefore, if a child has significant work of breathing, hypoxia, or other criteria qualifying possible admission, the clinician may consider a trial with one or both of the above medications.
Corticosteroids: not recommended for use in bronchiolitis in any setting. Use does not significantly reduce outpatient admissions or length of stay, and may actually prolong viral shedding in patients with bronchiolitis.
Oxygen Saturation: Oxygen saturation of 90% or above should be tolerated in infants and children with bronchiolitis, as no data exist to suggest such increases beyond 90% result in any clinically significant difference in physiologic function, patient symptoms, or clinical outcomes.
Chest Physiotherapy: not recommended, as no clinical benefit has been found by using vibration or percussion, or passive expiratory techniques. Deep suctioning is also not recommended, as it has been associated with a longer LOS in hospitalized infants 2 to 12 months of age.
However, external, noninvasive suctioning IS recommended, as studies have shown that lapses of greater than 4 hours in noninvasive, external nasal suctioning are associated with longer LOS.
Antibacterials: not recommended in bronchiolitis, as no benefit from use has been shown. Studies have shown that febrile infants without an identifiable source of fever have a risk of bacteremia that may be as high as 7%. However, a child with a distinct viral syndrome, such as bronchiolitis, has a lower risk (much less than 1%) of bacterial infection of the cerebrospinal fluid or blood.
Nutrition and Hydration: Clinicians should administer nasogastric or intravenous fluids for infants with a diagnosis of bronchiolitis who cannot maintain hydration orally; this accounts for approximately one third of hospitalized cases. No significant or statistical difference has been measured between use of formula via NG tube or dextrose containing IV fluids.
HAND HYGEINE – RSV can remain infectious on counter tops for ≥6 hours, on gowns or paper tissues for 20 to 30 minutes, and on skin for up to 20 minutes.
Hands should be disinfected before and after direct contact with every patient, after contact with inanimate objects in the direct vicinity of the patient, and before putting on and after removing gloves.
Use of palivizumab – see recommendations for age and disease history
Online version of this article available at: http://pediatrics.aappublications.org/content/early/2014/10/21/peds.2014-2742
Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and Management of Bronchiolitis. Pediatrics. The Official Journal of the American Academy of Pediatrics. 01 October 2006. Vol 188. No 4. Pages 1774 – 1793.
Online version of this article available at:
http://pediatrics.aappublications.org/content/118/4/1774.full
http://pediatrics.aappublications.org/content/early/2013/10/02/peds.2013-1501.full.pdf. Apnea in Children Hospitalized with Bronchiolitis. Pediatrics. The Official Journal of the American Academy of Pediatrics. Volume 132. No 5. November 2013.
Sepsis
Fever Work Up and Management in Infants
0-21 days
[table class=”table-striped table-col-border”]
Source,Well appearing and Low Risk2,Ill appearing or High Risk3 after initial labs
No Source,Full sepsis workup4\, LFTs\, CXR5 only if resp sx abx\, consider acyclovir6\, admit, Full sepsis workup\, LFTs CXR only if resp sx abx\, plus acyclovir\, admit
Bronchiolitis\, RSV\, Flu\, or other virus positive7,Full sepsis workup\, LFTs CXR only if resp sx abx\, consider acyclovir\, admit [attr colspan=”2″]
UTI8,Full sepsis workup\, LFTs CXR only if resp sx abx\, consider acyclovir\, admit [attr colspan=”2″]
[/table]
22-28 days
[table class=”table-striped table-col-border”]
Source,Well appearing and Low Risk,Ill appearing or High Risk after initial labs
No Source,Full sepsis workup\, CXR only if resp sx abx\, admit, Full sepsis workup\, +/- LFTS CXR only if resp sx abx\,consider acyclovir\, admit
Bronchiolitis\, RSV\, Flu\, or other virus positive,Full sepsis workup\, +/- LFTS CXR only if resp sx abx\,consider acyclovir\, admit[attr colspan=”2″]
UTI,Full sepsis workup\, CXR only if resp sx abx\, admit [attr colspan=”2″]
[/table]
29-56 days
[table class=”table-striped table-col-border”]
Source,Well appearing and Low Risk,Ill appearing or High Risk after initial labs
No Source, Urine4\, blood4\,
If Low risk\, no abx\, discharge and ensure follow-up
Admit if SBI – and refer to High Risk section, Full sepsis workup\, admit\, abx
Bronchiolitis\, RSV\, Flu\, or other virus positive, Urine\, blood\, If Low risk\, no CSF\, no abx\, discharge and ensure follow-up.
Admit if SBI– and refer to High Risk section
Or admit if needed for bronchiolitis with no abx, Full sepsis workup\, admit\, abx
UTI,Full sepsis workup\, admit\, abx[attr colspan=”2″]
[/table]
2-24 months
[table class=”table-striped table-col-border”]
Source,Well appearing and Low Risk,Ill appearing or High Risk after initial labs
No Source, Consider urine (see risk factors9), Treat per established clinical guidelines
Bronchiolitis\, RSV\, Flu\, or other virus positive, Consider urine (see risk factors), Treat per established clinical guidelines
UTI8,Consider initial IV treatment:
Infants < 6 months of age
Moderate / Severe Dehydration
Vomiting\, inability to tolerate oral fluids\, antibiotics
Concern for follow-up[attr colspan=”2″]
[/table]
Intitial Antibiotic Coverage (at meningitis doses)
[table]
0-21 days,Ampicillin/Cefotaxime (alt: Amp/Gent) +/-Acyclovir, GBS\, enterococcus\, GNRs\, HSV\, Listeria
22-28 days,Ampicillin/Cefotaxime (alt: Amp/Gent), GBS\, enterococcus\, GNRs\, Listeria
29-56 days,Cefotaxime (alt: Ceftriaxone ),Late GBS\, Pneumococcus
[/table]
Consider Vancomycin ((MRSA, resistant pneumococcus) if
- Ill Appearing
- Gram positive organism on Gram stain of blood or CSF
- CSF WBC > 8 and abnormal glucose or protein
Disposition (0-56 days) after admission10
Well appearing infants with no clinical concern for HSV and Blood, Urine, CSF Cultures NEGATIVE and
UA NORMAL
Discharge after 24 hours of negative cultures if: CSF Profile NORMAL, CSF Gram Stain NEGATIVE HSV CSF PCR NEGATIVE, if sent or Enterovirus Meningitis positive
Discharge after 36 hours of negative cultures if:
Uninterpretable LP/Bloody tap
PCR studies pending or not sent
For Ill appearing patients, other concerns, or other positive results, follow established guidelines
When to consider a blood culture upon initial evaluation beyond 0-56 days
- Ill appearing or toxic at any age
- At risk medical conditions (oncology, sickle cell, etc)
- Incomplete Immunizations
In general well appearing infants without risk factors are at low risk for bacteremia
Footnotes
1Fever – documented / history of rectal / axillary temperature ≥ 38°C (100.4) in the ED, at home, or referring MD’s office
2 Low risk Criteria
29-56 days old
Full-term (≥37 weeks gestation)
No prolonged NICU stay
No chronic medical problems
No systemic antibiotics within 72 hours
Well-appearing and easily consolable
No infections on exam
Blood:
WBC ≥ 5,000 and ≤ 15,000
Band to neutrophil ratio < 0.2
(Bands/bands + neutrophils)
Urine:
WBC < 10 /HPF
Negative Gram stain
Chest x-ray (if obtained):
No infiltrate
3High Risk
Do not meet the low risk criteria
If data is incomplete (urine or blood could not be obtained)
4 Labs
Blood – CBC with diff. Blood culture. LFTs if < 21 days or 0-28 days or up to 28 days if indicated for HSV suspicion
Urine –Cath UA w/ micro (at MFSMC= urinalysis complete) plus Urine culture
CSF – culture and gram stain (tube 1), protein and glucose (tube 2), Cell count and diff (tube 3), Viral studies or save (HSV PCR 0-28 days, Enterovirus PCRbetween June and November or CSF pleocytosis)
Respiratory Viral Panel for all admitted 0-56 day old patients year round
Full Sepsis workup = all of the above.
Blood culture bottles are placed in the main incubator at MFSMC at the time they are logged in by the main lab into medconnect. The machine reads every 10 minutes. A negative culture is real time
5 Consider CXR
Concern for bacterial pneumonia
Suspected HSV infection with respiratory symptoms
Suspected Chlamydia or Pertussis
6 When to consider HSV
Consider empiric HSV testing and treatment
Infants Option A – ALL < 21 days
Option B – < 21 days plus any of the following.
Mom had active primary HSV at delivery
Skin vesicles
Seizures, abnormal neurologis status
Elevated Liver Enzymes
CSF Pleocytosis – (especially if also CSF RBCs)
Infants 22—40 days and one of:
Ill Appearing
Abnormal neurologic status, seizures
Vesicular rash
Hepatitis
Mom known to have primary HSV infection at delivery
Infants 22-28 days
Additional:
For concern or dx of HSV, additional w/u includes
SEM (Skin, Eye, Mouth)
Add swabs from conjuctiva, buccal mucosa, rectum and any vesicular lesions
Disseminated Disease
Add BMP, LFTs, PT/PTT, type and screen, chest x-ray
7 Bronchiolitis
29-60 days with clinical bronchiolitis (with or without RSV) are at significantly lower risk for bacteremia and meningitis, but 3-5% rate of UTI
8 UTI
29- 60 days -positive bacteremia risk. Rare meningitis (usually ill appearing)
9 UTI risk factors ages 2-24 months (risk increases w number of risk factors
-Girls– non-black, T >39 C, Fever > 2 days, no other source, < 12 months, prior UTI -Male – Uncircumcised, non –black, T >39 C, Fever > 24 hours, no source, < 6 months, prior UTI
10 Byington et al.
Admitted culture negative infants at LR for SBI or at HR who test positive for a viral pathogen are eligible for dc at 24 hours. All other culture-negative infants are eligible for the same at 36 hours. Result: decr LOS, decr ABX use, decr cost with no change in readmission rate and no cases of missed SBI after hospital discharge.
CHOP Clinial Pathways. EDPathway for Evaluation and Treatment of Febrile Young Infants 0-56 days old. No. 2015
CHOP Clinical Pathways. Inpatient Pathway for the Treatment of Febrile Young Infants. Feb 2014